Lymph Node Removal: Why It's Important
- Staging Cancer: Guides treatment decisions.
- Guiding Treatment: Informs chemotherapy or radiation.
- Monitoring Outcomes: Tracks treatment effectiveness.

As you embark on the journey of understanding mastectomy procedures, consider the pivotal role that lymph node removal plays in your treatment. This surgical decision provides vital insights into cancer spread and significantly influences your recovery process. Are you ready to explore the nuances of this critical aspect of surgery?
Understanding the connection between different mastectomy types and the necessity of lymph node removal is crucial for informed decision-making during breast cancer treatment.
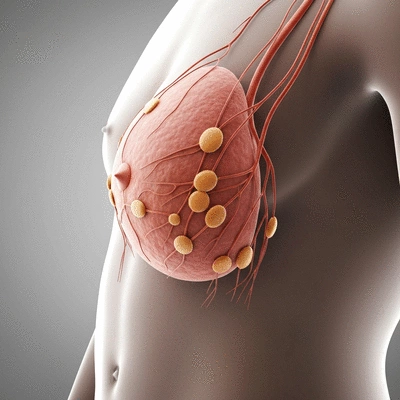
When discussing mastectomy procedures, it’s vital to understand the role of lymph node removal. This aspect can significantly influence your recovery and overall treatment success. Lymph nodes are small, bean-shaped structures that help filter harmful substances and are key players in your immune system. During a mastectomy, healthcare providers may recommend lymph node removal to assess the extent of cancer spread. Research published in PMC NCBI highlights the evolving understanding of lymph node management in breast cancer, emphasizing that the decision for removal is tailored to individual patient needs and cancer characteristics.
By removing lymph nodes, we can determine if cancer has invaded these critical areas, which is essential for tailoring your treatment plan. This information provides insights into your cancer stage and can guide further therapies. Are you curious about how lymph node removal impacts different types of mastectomy? Let’s delve deeper!
Lymph node removal, also known as lymphadenectomy, is a surgical procedure where one or more lymph nodes are excised. This process is important for several reasons:
Understanding *why* this procedure is performed can empower you as a patient. When you know what to expect, it can ease some of the anxiety surrounding surgery.
The type of mastectomy you undergo can dictate whether lymph nodes will be removed. For instance, in a modified radical mastectomy, surgeons typically remove several lymph nodes to evaluate cancer spread. In contrast, a simple mastectomy might involve less extensive lymph node removal. Recent studies, such as one featured in Nature.com, demonstrate how advanced imaging techniques are improving the precision of lymph node assessments, potentially reducing the need for extensive surgical removal in some cases.
As I guide patients through their options at the Mastectomy Insight Hub, I emphasize the importance of discussing these connections with your surgeon. It’s essential to understand how these decisions will impact your treatment pathway and recovery.
Now that we’ve established the significance of lymph node removal, it’s time to explore the various types of mastectomy and the specific lymph node techniques associated with each. This information is crucial as it can help you make informed decisions about your surgical options.
A simple mastectomy, or total mastectomy, involves the removal of all breast tissue but typically does not require lymph node removal unless there is a prior indication of cancer. Here’s what to expect if lymph nodes are part of your procedure:
This approach can be ideal for patients who are at low risk for lymphatic complications or have specific cancer profiles.
The modified radical mastectomy removes the entire breast along with some lymph nodes from the armpit area (axilla). This technique is often utilized for patients with a confirmed diagnosis of breast cancer.
It’s important to discuss with your healthcare team the implications of lymph node removal during this procedure, so you can feel confident in your surgical journey.
In a radical mastectomy, not only is the entire breast removed, but most of the nearby lymph nodes are also excised. This procedure is usually reserved for more advanced cancers.
Understanding the necessity and implications of this approach is key to navigating your recovery effectively.
Both skin-sparing and nipple-sparing mastectomies aim to preserve as much breast skin as possible, which can enhance cosmetic outcomes. However, they can still involve lymph node removal depending on the cancer diagnosis.
As you consider your options, engaging in a conversation with your surgeon about how lymph node removal will fit into these types of mastectomy is essential for making informed choices.
Finally, it’s crucial to understand the collaborative role of oncologists and breast surgeons in your treatment plan. These professionals will evaluate your unique situation, discussing the necessity and type of lymph node removal based on your cancer diagnosis.
Having an open dialogue with these experts can help you feel prepared and confident in your decisions as you navigate this critical aspect of your healthcare journey.
Lymph node removal is primarily performed to determine the stage of cancer and assess if it has spread beyond the breast. This information is crucial for guiding further treatment decisions, such as chemotherapy or radiation.
The extent of lymph node removal depends on the type of mastectomy. A simple mastectomy may not involve lymph node removal unless cancer is indicated, while a modified radical mastectomy typically includes removal of some lymph nodes. A radical mastectomy involves comprehensive lymph node removal, usually for more advanced cancers.
One of the main potential risks is lymphedema, a condition causing swelling in the arm due to fluid buildup. Other risks include pain, numbness, and limited arm mobility, which can often be managed with physical therapy and other supportive care.
It is important to discuss the purpose of lymph node removal in your specific case, the techniques that will be used, potential risks, and the expected impact on your recovery and long-term health. Also, inquire about financial considerations and insurance coverage.
In some cases, less invasive techniques like sentinel lymph node biopsy (SLNB) may be used. SLNB involves removing only a few lymph nodes to check for cancer spread, potentially reducing the risk of lymphedema compared to full axillary lymph node dissection.
Did you know? Engaging in a pre-surgery consultation with your healthcare team about lymph node removal can significantly enhance your comfort level. Prepare a list of questions regarding the procedure, recovery, and potential impacts on your treatment plan. This proactive approach can empower you and help alleviate anxiety as you navigate your surgical journey.
Preparing for your mastectomy can feel like a daunting task, but it’s essential to approach it with confidence and clarity. Many patients, including myself, have found that gathering information about the procedure, especially regarding lymph node removal, can significantly reduce anxiety. Let’s explore some real patient stories and insights that may help you feel more informed as you embark on this journey!

Hearing from others who have walked the same path can provide comfort and guidance. Many patients share their experiences with lymph node removal, emphasizing the importance of understanding what to expect:
These stories highlight the shared experiences that can ease your mind. Remember, you are not alone—many have successfully navigated this journey!
Equipped with the right questions, you can engage more effectively with your healthcare team. Here are some important questions to consider asking:
Having these conversations can empower you to make informed decisions about your care and ensure that your needs are addressed.
It’s important to understand the financial aspects of your surgery, including insurance coverage. Take the time to review your health insurance policy and discuss:
Understanding these details will help you prepare financially and reduce stress leading up to your surgery. If you have questions about navigating insurance, I’m here to help guide you through the process!
As you prepare for your mastectomy, it’s essential to reflect on your options and make informed decisions that align with your needs. Let’s dive into some key considerations that can help shape your surgical journey.
The financial aspect of your surgery shouldn’t be overlooked. Evaluating costs for lymph node removal can help you better understand your overall expenses. Here are several factors to consider:
By addressing these factors ahead of time, you can feel more prepared both financially and mentally.
Your decision on the surgical approach should be based on a thorough understanding of your specific situation. Factors to consider include:
Remember, it’s vital to communicate openly with your healthcare team to find the approach that feels right for you.
As you navigate your options, don't forget to explore clinical trials. They can offer access to the latest treatments and techniques, which may be beneficial for your situation. Consider discussing:
Participating in a clinical trial could open new doors for your treatment, offering hope and the opportunity to contribute to medical research.
Here is a quick recap of the important points discussed in the article:
Caring for Drains and Incisions

When it comes to recovery after a mastectomy, understanding the role of surgical drains can be both
Mastectomy Preparation: Key Instructions Explained

As you prepare for your mastectomy, understanding what lies ahead can transform uncertainty into con
Embracing Flat: Real Patient Stories

What if the journey after a mastectomy could be navigated with confidence and empowerment? Understan
Caring for Drains and Incisions
Mastectomy Preparation: Key Instructions Explained
Embracing Flat: Real Patient Stories
Patient Support in Mastectomy Recovery
Mastectomy Complications and Care Guide